Introduction
It is often said that there is no such thing as failure, only differing degrees of success. This sentiment is particularly relevant in endodontic care, in that it highlights the challenges of defining treatment success objectively. In endodontology, the primary goal is to attain and preserve the health of the periapical tissues. Outcome measures have been incorporated into endodontics for decades to analyse whether this objective has been achieved, thereby documenting treatment effectiveness, evaluating patient care, and facilitating decision-making. Outcomes may be subclassified into those reported by clinicians and those from the perspective of the patient.
While the delivery of endodontic care is patient centred, outcomes are rarely patient defined. The outcome of endodontic therapy has been traditionally examined from a clinical perspective, with adjunctive imaging technology. Outcome measures have prioritised the technical and clinical aspects of treatment, with little emphasis on the patient perspective. With the advancement of a patient-centred model of healthcare in recent decades, the focus of outcomes has changed. There has been an emerging interest in measures that complement the classic goal of endodontics from the patient’s perspective. These are termed patient-reported outcomes (PROs).
Despite the increasing volume of outcome research, there is currently a lack of studies relating endodontic therapy to these aforementioned outcomes.1 Recently, endeavours to develop a core outcome set (COS) for endodontics have culminated in several publications on outcome reporting in systematic reviews.2,3 However, there remains a lack of consensus on a unifying criterion for endodontic outcomes, with clinicians, researchers, and patients all contributing differing ideas of what constitutes success.
The objectives of this review are to explore the current use of PROs in endodontology, establish the potential value of including these measures in future endodontic care and research, and to examine the necessary prerequisites for their adoption into a COS for endodontics.
Outcomes: their role in delivery of care
Endodontic therapy encompasses a range of treatment modalities, including nonsurgical and surgical treatments, vital therapies and retreatment procedures. The principal aim of treatment is the prevention or elimination of pulpal and/or periapical disease, to ensure the health of the periradicular tissues and tooth retention. There is a strong focus on outcomes of care in endodontics to determine whether a treatment has been successful in achieving the aforementioned objectives.
Outcomes may constitute any consistently anticipated, measurable consequence of treatment to assess the effectiveness of one therapy over another. Outcome analysis is determinant to substantiate patient decision-making when endodontic therapy is weighed against alternative treatment options. Consequently, the availability of pooled data within the literature is used to reassure the public in relation to the validity of endodontic treatment. Therefore, a clear definition of success and failure is essential when considering endodontics as a valid treatment option for a tooth with pulpal and/or periapical disease.
How successful is endodontic therapy?
The outcome of endodontic treatment can be examined across four distinct dimensions: clinical (absence/presence of disease/pain); tooth longevity; economic; and, psychological, e.g. quality of life/satisfaction.4 Endodontology has traditionally used proxy clinical and radiographical parameters, based on a defined referential comprising clinical and biological data collected about patients by clinicians. Success or failure has been decided based on specific clinical findings, in conjunction with radiographic evidence of a healing periodontium.
A range of terminologies and instruments have been proposed to describe successful root therapy, including strict and loose criteria based on radiographical healing of the periradicular tissues, used by Strindberg’s dichotomous system, to dictate success. Given the ambiguity of terminology in the past, the terms ‘favourable’, ‘unfavourable’ and ‘uncertain’ are currently preferred, in line with contemporaneous guidelines. Based on the aforementioned criteria, endodontic therapy presents an efficacious treatment option.
Limitations of current measures
Clinical outcomes predominate in the literature when assessing the effectiveness of endodontic therapy. A recent scoping review found that only 3% of studies included PROs as primary outcomes of endodontic care.5 Clinician-reported outcomes (CROs) alone often fail to encapsulate the functional and physiological impact of endodontic disease and its treatment on the patient. While clinicians can make objective observations regarding the effectiveness of endodontic treatment, it is the patient who can most accurately report on how treatment has impacted their life. Patients are unlikely to be aware of the pathophysiology of endodontic disease, but are sensitised to treatment-related factors, alongside concerns over retaining a functional tooth. Consequently, these traditional CROs appear to be more relevant to clinicians and researchers than they are to patients.
Additionally, clinical outcomes fail to adequately capture patients’ experience, from the care they receive to its effect on their oral health and quality of life. The patient, even in the absence of objective signs of treatment failure, may be dissatisfied with the treatment outcome if pain or other features are present. Clinical and radiographic criteria may be irrelevant to patients, who may base their idea of success on personal values and expectations, rather than the presence of healing periradicular tissues. Indeed, even radiography to assess periapical healing has its limitations, with one study concluding that different evaluators agreed on a diagnosis less than 50% of the time.6 Therefore, clinical and radiographic measures should not be used as the sole means of analysing endodontic outcomes.
A changing perspective on health
The traditional view of oral health has changed over the years, from a narrow, reductive perspective, to one that recognises how oral health impacts daily living. The biomedically oriented, paternalistic view is being replaced by a more patient-centred approach, with emphasis on the disease process within the wider context of health.7 This has led to a paradigm shift in the delivery of oral healthcare to assess treatment needs and outcomes from a patient’s perspective, rather than relying on the perspectives of clinicians alone. The World Dental Federation (FDI) has emphasised that endodontic disease should be considered within the greater context of health, a concept known as endodontic medicine.8 The adoption of a patient-centred approach in endodontology aims to eliminate disease, alleviate pain, restore function, and improve quality of life, representing a multifaceted, modern approach to care.
Patient-reported outcomes
Assessment of treatment outcomes from a patient perspective is an integral component of evidence-based practice, as it is linked to patients’ expectations from treatment. Clinicians often focus on short-term outcomes by providing treatment, rather than providing overall health outcomes through patient-centred care. Considering the views of the patient may serve to complement or even challenge the viewpoint of clinicians.
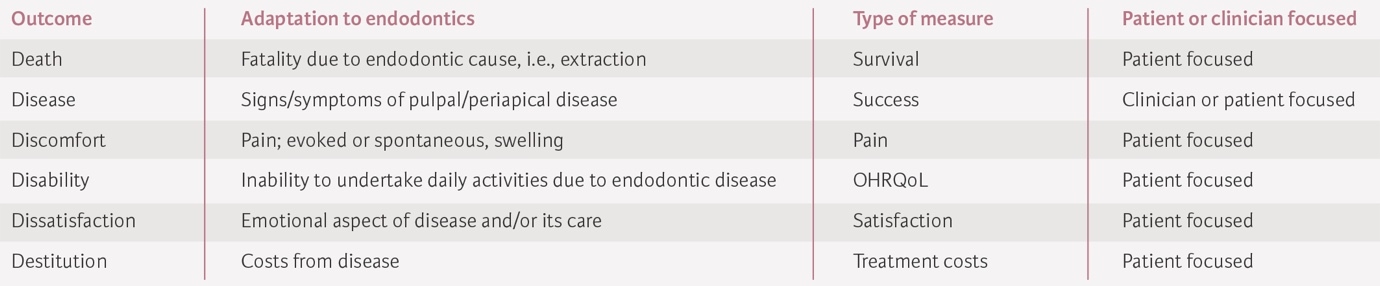
Outcomes reporting on the status of patient health, without interpretation by a clinician, are known as PROs. PROs include a broad range of measures but commonly reflect tooth survival, quality of life (QOL), function and pain. Such outcomes are also likely to consider patient expectations, alongside their desire to participate in their care. The European Society of Endodontology has published a consensus document to highlight appropriate outcomes to assess the effectiveness of endodontic therapies, in a bid to develop the S3-level clinical practice guidelines for the management of pulpal and periradicular diseases (Table 1).
Patient-reported outcomes in endodontics
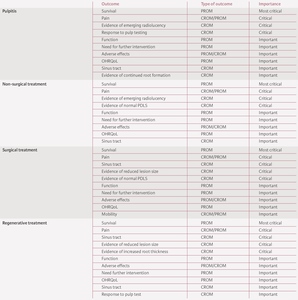
There has been a growing interest in the field of endodontic research regarding patient perspectives on treatment and how oral disease can affect an individual’s life.9 While PROs have been researched extensively in healthcare, they have only become of interest in endodontics in the last two decades. According to Azarpazhooh et al., the number of PRO studies has increased from a single study in the 1990s to equate to 36% of all outcome-based endodontic research in the 2010s.5 To assist in systematic review reporting, recent online Delphi surveys were conducted to ascertain outcomes relevant to endodontics from the clinical and patient perspective, and their relative importance was ranked.10
Tooth survival and function
Tooth survival has been reported as the most critical outcome in endodontics. A tooth is said to have survived if it remains as part of the dentition while maintaining functionality.11 Survival rates for endodontics are uniformly high in the literature (Table 2). Even with some persistent disease, if a tooth is asymptomatic and functional, the patient may deem this a success, and may opt not to have further treatment completed, highlighting patient autonomy in setting less demanding goals for treatment. The impact of accepting a tooth with periapical disease is unknown, and more research is needed concerning the risks associated with retaining such a tooth. Despite its importance, the representation of this outcome in the literature is low.5
Pain, tenderness and need for medication
Preoperative pain is the main driving factor that influences a patient’s decision to seek treatment and is the most consistently reported PRO in the literature.24 As such, attaining a pain-free tooth often overrides all other considerations for the patient. Therefore, postoperative pain is a critical outcome to consider. While pain is an important factor to consider in treatment planning, it is arguably the impact this has on a patient’s daily life that is of most relevance to understand disease burden and the benefit endodontic therapy can provide.
Quality of life
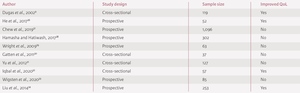
Quality of life (QoL) has been reported as an ‘important’ PRO to consider in endodontics. Endodontic pathology has been associated with a diminished oral health-related quality of life (OHRQoL),25 due to pain/loss of function. Endodontic interventions have been shown to significantly benefit patients’ QOL across all endodontic subspecialties.26 Similar levels of OHRQoL improvement are reported where endodontic care is contrasted with other interventions in the primary care setting.27 However, this is not a consistent finding in the literature (Table 3). The impact of adverse effects of endodontic treatment, e.g., discolouration/allergies, on QoL should also be considered.
Expectations/satisfaction
While not considered in the recent working group consensus, meeting patient expectations is a fundamental element of patient-centred care. Endodontic therapy has high reported rates of satisfaction, with specialist care having higher satisfaction than treatment in general practice.28 Certain factors have been linked with dissatisfaction, such as costs and duration of treatment. Overall, a limited number of studies consider patient satisfaction as an outcome of treatment.
How PROs can benefit clinicians and patients
The selection of appropriate PROs is crucial in the bid for patient empowerment within endodontics and in the formulation of positive care outcomes. Emphasising the psychosocial well-being of patients results in a shift from disease treatment to improving a patient’s overall well-being.
In the delivery of holistic, patient-centred care, some authors believe that the patient is in the ideal position to evaluate the care they have received, with some disputing the relevance of clinician-reported outcomes.35 While persistent disease from a biological standpoint may represent a failure, a functional, asymptomatic tooth may be seen as successful to the patient. One study found that 97% of a cohort who had received endodontic treatment were satisfied with their treatment, even though 96% had evidence of disease present.9 While the foremost goal of endodontic therapy should be the treatment of apical periodontitis, the decision to instigate further interventions must be mutually decided with the patient, with consideration for personal values, risks and monetary concerns. Success is said to be in the eye of the beholder, and PROs may serve as a normative guide to the clinical action that should be taken in the presence of emerging/persistent disease.36 This must be carefully considered alongside the risk of future disease progression.
PROs may help clinicians to understand patient expectations from treatment, which is necessary to ensure that clinician and patient goals are aligned, leading to increased satisfaction and improved clinical outcomes. Research has demonstrated that considering the feedback obtained from patients relating to the outcomes of care can improve adherence to treatment and post-treatment instructions.37 While practitioners may strive for complete healing, patients often set less demanding expectations once they can retain the tooth without pain. Therefore, patient-centred care allows clinicians to holistically evaluate the appropriateness of different treatment options in light of the patient’s needs and values.
For a tooth that requires endodontic therapy, a range of options exists outside the realm of endodontic therapy. PROs may facilitate appropriateness in the treatment option chosen when consideration is made for factors beyond cost, such as complexity and the benefits to QoL from the preservation of the natural dentition.
The development of a core outcome set for endodontics
The implementation of evidence-based practice into the clinical setting requires integrating results from high-quality primary research. To overcome the emphasis on technical, clinician-focused outcomes, there has been interest in the formulation of an agreed set of standardised outcomes in endodontic trials, as seen in other areas of dentistry.38 The importance of a COS has been highlighted by the Grading and Recommendations, Assessment, Development and Evaluation (GRADE) group, an international system that assesses the evidence and quality of healthcare research, to form the basis for recommendations in endodontics.
While a limited COS has been published as part of the S3-level clinical practice guidelines development process, recent endeavours have seen the publication of an a priori protocol to reach a consensus on the most critical outcomes to consider in endodontic care, alongside how best to measure them and intervals for their follow-up.39 The critical aspect of this COS is that the patient is the primary focus, thereby highlighting outcomes that may not have been identified previously. Considerations for PROs at the centre of the COS will bring greater attention to patient-related domains in the future, allowing the formulation of more meaningful, evidence-based conclusions, with an emphasis on the impact of endodontic therapy on patients.
Future challenges
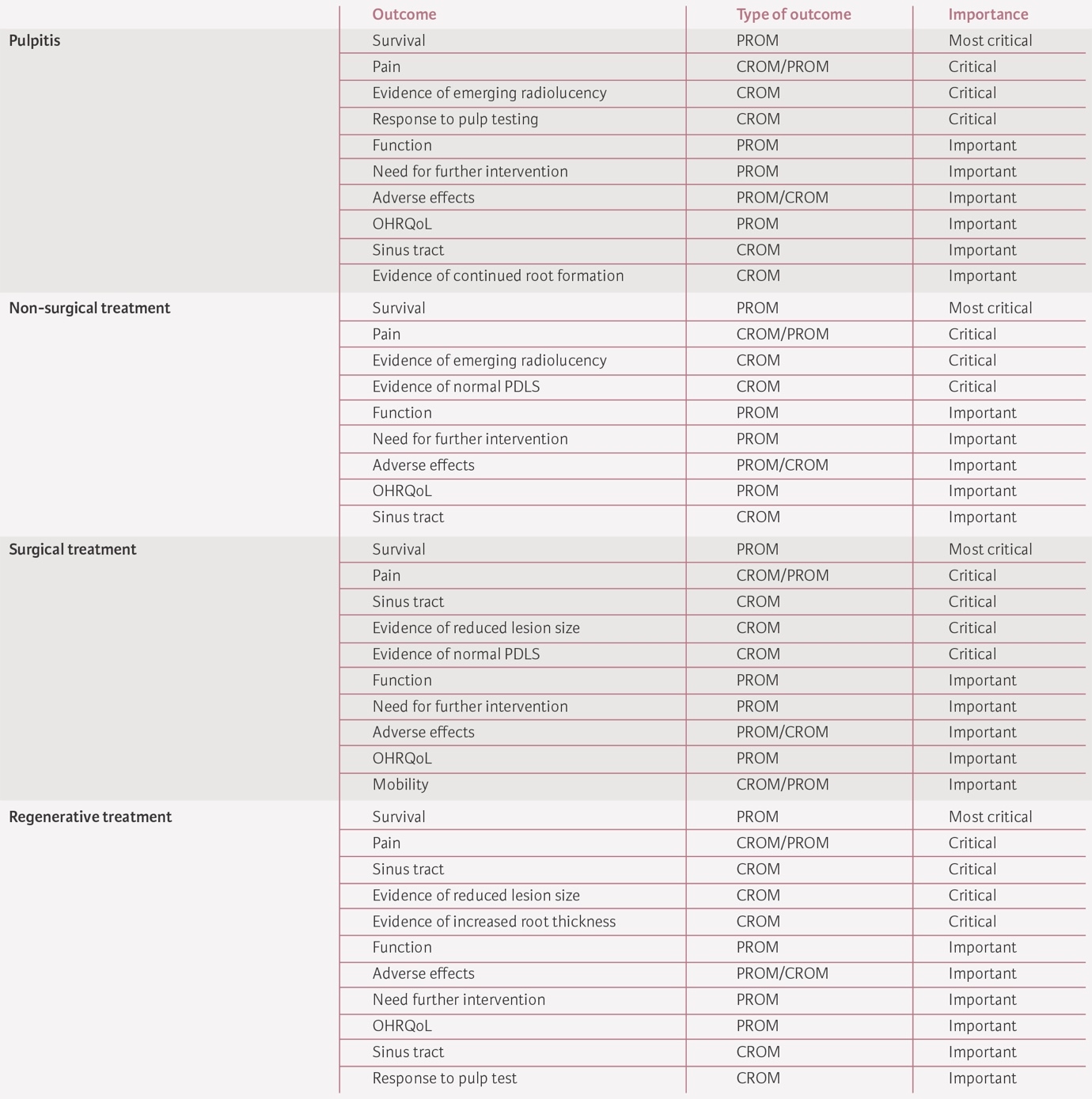
There is a need for sensitive instruments to accurately measure specific PROs, which can discriminate between patients with and without endodontic problems, as well as differences in PROs pre and post treatment. Current instruments, such as the Oral Health Impact Profile 17 (OHIP-17) for QoL, lack the necessary validity and sensitivity to allow comparisons to be made between studies. Alongside the use of ad hoc instruments, the lack of standardisation between studies precludes reliable comparisons from being made.40 To improve reporting consistency, some authors have proposed assigning outcomes to specific domains using the 6D model (Table 4).5 The implementation of disease-specific, multi-dimensional, standardised measures may be required before the inclusion of PROs within the COS for endodontics.41
Discussion
Outcomes have been an integral component of endodontic therapy for decades. The purpose of analysing a defined set of outcomes is to ascertain treatment effectiveness and quality of care. Patients cannot make informed decisions on which therapy to choose without being afforded information regarding the expected outcomes from that treatment. The selection of well-established outcomes is critical in the current age of evidence-based dental care, allowing clinicians to make, defend and analyse clinical decisions, together with the patient. Consideration of PROs may result in an improvement in the quality of care, as well as enhancing the effectiveness of treatment interventions.42
The upsurge of evidence-based, patient-focused practices has prompted the endodontic community to reconsider outcomes of care. While clinician-focused measures are still necessary, the importance of patient-reported measures has become more apparent in recent years. Current evidence has demonstrated improved outcomes of care when these measures are employed alongside clinician-based outcomes.
Despite its importance, no core outcome set for endodontic treatment (COSET) currently exists. The selection of relevant outcomes is essential for the formulation of practice guidelines and for conducting systematic reviews of the literature using the GRADE framework.43 Adapting current models to incorporate the COSET to include clinician-based and patient-reported outcomes is fundamental in the modern era of evidence-based endodontic care, as the patient is recognised as a key stakeholder in future guideline development.10 With the inclusion of PROs in outcome reporting, their use is likely to increase, providing valuable information in relation to their benefit in the delivery of endodontic care in the future.
The scarcity of studies investigating PROs is problematic. Integrating PROs into future outcome studies may tailor research questions toward patients and report on those aspects that hold value for them.44 Additionally, the current state of instruments to measure PROs is insufficient to facilitate comparisons between studies. Valid, sensitive instruments may be necessary before the analysis of PROs can become more mainstream.
Conclusion
Outcomes in endodontics have advanced from the dogmatic criteria of Strindberg towards a patient-focused model, with an emphasis on the elimination of symptoms and ensuring tooth survival, even if some areas of periapical disease remain present. A comprehensive, evidence-based approach to assessing endodontic outcomes should consider the judicious selection of PROs, alongside well-validated, clinician-based views, in the bid for patient empowerment, satisfaction with care, and enhanced health outcomes.
.jpeg)

.jpeg)