Introduction
Facial infiltrating lipomatosis (FIL) is a rare congenital condition first described by Slavin in 1983.1 The major morphohistological characteristics of FIL include mature non-encapsulated adipocytes penetrating neighbouring structures (e.g., masseter muscle, parotid),2 benign proliferation of adipocytes, absence of lipoblasts, increase in numbers of vessels and nerves, and adjacent bone hypertrophy. Facial asymmetry is typically observed at birth and progresses with growth.3
Dermatological features are often the first to be noticed and include unilateral facial swelling with ipsilateral epidermal naevi of varying length, hypertrichosis, thickened lips, and capillary blush.4 Oral features ipsilateral include ipsilateral hemimacroglossia, unerupted teeth, hypodontia, mucosal neuromas, and macrodontia.2,3,5
Advances in sequencing technology have demonstrated the link between somatic phosphatidylinositol 3-kinase catalytic subunit alpha (PIK3CA) pathogenic variants and numerous overgrowth disorders (PIK3CA-related overgrowth spectrum or PROS).5 PIK3CA mutations result in cell hyperproliferation6 and have been identified in FIL patients.7 Localised and segmental lesions like FIL are associated with hotspot PIK3CA variants, whereas systemic disorders that would be the main differentials, such as CLOVES syndrome (congenital lipomatous overgrowth, vascular malformations, epidermal nevi, and skeletal/scoliosis and spinal abnormalities) and MCAP (megalencephaly-capillary malformation-polymicrogyria), are more likely to be caused by non-hotspot and rare PIK3CA variants.2
Medical background
We present the case of a male infant born at full term by elective caesarean section at 39 weeks’ gestation who exhibited a right-sided facial swelling soon after birth. The swelling appeared to be asymptomatic and there were no associated feeding difficulties. An increase in size of the swelling was noted at a four-week assessment by the paediatric medical team.
Dermatological features
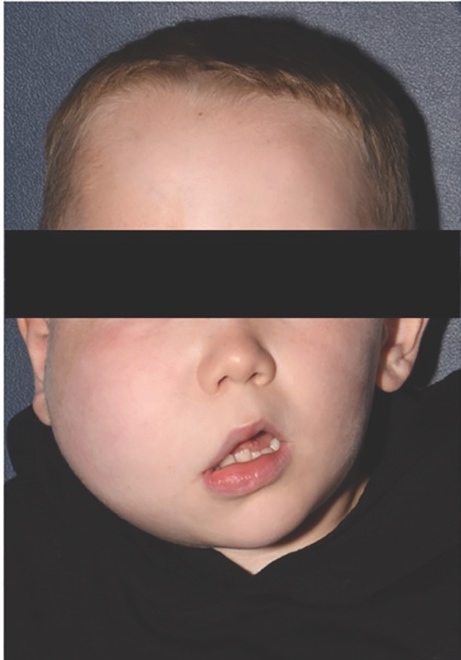
In addition to the right cheek swelling, a faint linear hyperpigmentation of the right cheek was noted by the paediatric dermatology team. This was initially localised to the pre-auricular skin but with time became more prominent on the cheek and forehead, and developed the classical appearance of an epidermal neavus. Subtle telangiectasia and mild hypertrichosis of the involved cheek also became more obvious over the first two years (Figure 1).
Investigations
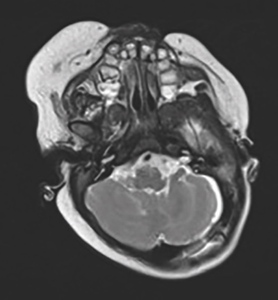
An ultrasound of the right cheek on day six post birth demonstrated a diffuse increase in subcutaneous fat within the cheek. No abnormal Doppler blood flow or cystic component was identified. A repeat ultrasound after eight weeks demonstrated an increase in size of the abnormality but with a similar radiological appearance. Magnetic resonance imaging (Figures 2 and 3) at 11 weeks demonstrated lipomatous hyperplasia of the right head and neck soft tissues including buccal, pre-auricular and submandibular region (Figures 2 and 3).
Imaging supported the clinical diagnosis of unilateral FIL, prompting genetic testing for a PIK3CA mutation. A sample from the right buccal mucosa confirmed a somatic mutation to PIK3CA (Figure 4).
Medical progress
In addition to the cutaneous presentation, the presented case has mild right-sided hearing impairment secondary to the surrounding tissue overgrowth and also anisometrophic hypermetropia and astigmatism in the right eye (managed by corrective glasses). He is otherwise doing well with no concerns of development delay. Now aged six, he is doing well at school following appropriate adjustments to his classroom environment for his mild hearing impairment. Due to the rare, complex nature of his diagnosis, he remains under the care of a number of medical specialties including dermatology, ear, nose and throat (ENT), and a plastic surgery team at a tertiary centre (Great Ormond Street Hospital). Surgical and medical (systemic PIK3 inhibitors) interventions may be required in the future; however, as he has remained relatively stable in recent years, a conservative approach is currently being taken.
Dental progress
This child has always presented with a clinically caries-free dentition, and healthy intraoral soft tissues with no obvious ulceration. The dental anomalies are coincident with the right side, where infiltrating lipomatosis is present.
At age 12 months, the child presented with hyperplasia of the upper right alveolar arch and premature eruption of the upper right primary canine, upper right first primary molar and lower right first primary molar (53, 54 and 84).
At age three years and seven months, the child presented with early loss of the lower right primary lateral incisor (LRB), mild midline discrepancy, right buccal crossbite and left lingual crossbite (Figure 5).
At age five years and seven months, the child presented with early mixed dentition, i.e., premature eruption of the upper right first premolar, upper right first permanent molar, lower right permanent central incisor, lower right permanent lateral incisor, and lower right first permanent molar (14, 16, 41, 42 and 46), mild hypoplasia upper right first premolar (14), moderate midline discrepancy – right centreline shift, incisal class III – edge to edge, right-sided buccal crossbite, and left-sided lingual crossbite (Figure 6).
Dental management of the child at present
Over 4.5 years, a prevention regime was implemented:
-
six-monthly attendance with the local community dentist;
-
22,600 fluoride varnish application every six months;
-
1,450ppm fluoride toothpaste with supervised brushing twice a day;
-
fissure sealants of the premature permanent dentition;
-
clinical photography to document occlusion;
-
annual review at the paediatric dental hospital for close monitoring; and,
-
an assessment in the hospital’s orthodontic department will be conducted around age nine, following further growth and development of the permanent dentition, to determine if orthodontic intervention is necessary.
No active dental treatment has been required as the child remains caries free.
Discussion
FIL is a unilateral congenital craniofacial deformity caused by adipocytes infiltrating surrounding facial structures. The most frequently affected structures are the parotid, tongue and masseter.8
Radiological investigations involve magnetic resonance imagining to demonstrate diffuse fatty infiltration and increased thickness of subcutaneous fat on the affected side, as a bright signal.8 Computed tomography typically shows a non-encapsulated diffusely infiltrating low-attenuation mass and changes to the facial bones.9
A case reported by Hongrui et al.2 describes a patient who had computed tomography reconstruction, which showed considerable zygomatic and mandibular enlargement and misalignment of teeth, resulting in an overbite and malocclusion. This case also describes ipsilateral hemimacroglossia with some unerupted teeth on the affected side.2 Also, observed features of the affected side include: abnormal root formation; early eruption of deciduous and permanent teeth9; hemimacroglossia; erythema; and, mucosal neuroma.3 FIL is predominantly asymptomatic but as it affects a patient’s appearance, it often impacts psychosocial well-being and facial functionality such as chewing, swallowing and vision.10
Pathophysiology
Genetic testing of samples obtained from FIL show PIK3CA to be the cause of soft tissue and bone overgrowth, as in this case report. The pathophysiology is not fully understood, especially why various cells, e.g., fat, bone, and endothelial cells with different embryonic origins, are affected.2 One theory is that the mutation occurs early in embryonic development before cell differentiation.2 Another theory is whether the mutated cells are affecting the surrounding cells through cell contact, cytokines or via other unknown mechanisms.2
Treatment
Surgical resection is the main form of proposed treatment, involving the resection of infiltration of adjacent tissue and osteotomy of skeletal hyperplasia.2 However, due to the complexity of FIL presentations, surgery is not always possible and pharmacological approaches are sought.2 Surgery carries the risk of recurrence and damage to vital anatomical structures.9 Surgery should ideally be performed at the end of the facial growth period.11 Facial growth typically concludes around the age of 17 for females and around 21 for males.12 Parents of children with FIL may request early surgery for aesthetic and self-esteem issues that may become evident during the school years. However, due to the increased activity of the growth hormone prior to facial growth completion, the recurrence rate is likely to be increased.3 The delay of definitive surgery has advantages such as minimising the chance of damage to the facial nerve, decreasing the total number of procedures, and having a mature contralateral cheek contour to match.11 Liposuction can be attempted depending on the size of the lesion. Drug approaches utilise PIK3K-targeted inhibitors, which aim to reduce the lesion volume, thus improving function. Alpelisib is a PI3K-selective inhibitor13 and studies have shown a significant reduction in volume of facial soft tissues after one month. Notably, the drug does not affect skeletal deformities.10 Further prospective studies are required to investigate side effects, optimal treatment duration and dosage for age groups, and the possibility of relapse after drug withdrawal.2
Conclusion
FIL presents as a unilateral facial swelling that often presents at birth and slowly grows with age. Dermatological manifestations are the first noticeable signs and such patients need a thorough dermatological assessment to rule out systemic or syndromic associations. It is important that these patients are seen promptly and referred to other specialties appropriately and early. The associated dental anomalies require close monitoring and intense prevention advice to prevent decay to the prematurely developing dentition or the limited dentition if hypodontia is observed. Clinical examination, radiographical imaging and genetic testing aid diagnosis. The medical management is multifaceted with regular bi-annual or annual reviews depending on the specialty due to the potential involvement of several organs. Paediatric dentistry conducts an annual review of the child, in collaboration with the community dental services, to ensure comprehensive shared care. Multidisciplinary management is therefore crucial. Surgical and medical (PIK3 inhibition) treatment may be required in individual cases depending on the severity of overgrowth and associated complications.



.jpeg)
.jpeg)



.jpeg)
.jpeg)